Mechanisms of respiratory failure (hereafter referred to as RF) relating to pulmonary blood flow disorders are rarely isolated: more often RF proceeds according to the disorder type of the ventilation-perfusion relations, but even in these situations, mechanisms of pulmonary blood flow disorders can predominate.
Pulmonary blood flow has many differences from the circulation in greater circulation. First of all, there are two circulatory systems in the lungs: the bronchial blood flow, firstly described and drawn by Leonardo da Vinci in 1513, not different from the blood flow of the other organs and tissues, and the pulmonary — the so-called lesser circulation, which differs significantly from the greater circulation. There are anastomoses between them, both under normal and especially under pathological conditions.
Pulmonary blood flow disorders leading to RF can be of three types.
In case of the first type, there can be a pulmonary blood flow disorder due to macro- and micro-embolism by thrombotic masses, fat, amniotic fluid or gas. The mechanisms relating to this type of disorder depend on the nature of the embolism and can cause pulmonary ischemia, reflex phenomena in the lesser and greater circulation as well as the bronchi and finally act on the alveolar tissue by the biologically active substances released from the emboli.

Fig.1. Localization of emboli of the pulmonary artery and their manifestation [1, p. 124]
The second type of disorder is pulmonary vasculitides, which cause mainly ischemia of the lung. This group of pathological disorders of pulmonary blood flow is quite large and includes Wegener’s granulomatosis, allergic angiitis, Takayasu arteritis (usually affects large branches of the pulmonary artery and the aorta), hyperreactive vasculitides like Schoenlein-Henoch disease, septic diseases. Some of these vasculitides affect the whole body, but firstly the lungs are involved in the process because their vasculature is so large, allergens can enter them from the air and, also the lungs are particularly full of cells that produce vasoactive substances.
The third type of pulmonary blood flow disorder causing RF is pulmonary arterial hypertension, which can result from the acquired mitral valve diseases and congenital heart defects, thromboembolism, COPD; it can be primary or idiopathic. It is associated with pathology of pulmonary feltwork (plexogenic pulmonary arteriopathy) and with low-flow pathology. One of possible causes of pulmonary hypertension is hypoxia. Pulmonary hypoxic hypertension occurs in the case of mountain sickness, COPD, fetus and neonatal diseases, pregnancy and other conditions.
Lung perfusion disorder is a typical form of pathology of the external respiratory system, pathogenetic basis of which is inadequacy of the total capillary blood flow in the lesser circulation to the volume of alveolar ventilation in a period of time.
Among the causes of lung perfusion disorders are the following:
- Circulating blood volume
- The operating effect of the right and left ventricles of the heart
- Pulmonary vascular resistance
- Interalveolar air pressure
- Effect of gravity
Significant lung perfusion disorders occur in case of the hypo- and hypertension in the vessels of the lesser circulation (pulmonary hypo- and hypertension).
Pulmonary hypertension:
Pulmonary hypertension is an increase in pressure in the vessels of the lesser circulation. It can be caused by the following factors:
- the Euler-Lilestrand reflex
- blood flow reductions
- alveolar pressure increase
- blood viscosity increase
- cardiac output increase
- biologically active substances are produced under the influence of hypoxia in the lung tissues
- defects of the left heart compartments, arterial hypertension, ischemic heart disease, etc. [2, p. 195]
There are three forms of pulmonary hypertension: precapillary, postcapillary and mixed (Fig. 2).
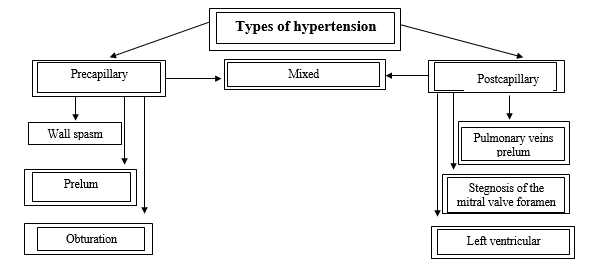
Fig. 2. Main types and causes of hypertension of the lesser circulation [3, p. 214].
Precapillary hypertension
It is characterized by an increase in pressure in pre-capillary and capillary above normal (over 30 mmHg systolic and 12 mmHg diastolic) with a decrease in blood flow in the pulmonary artery system.
The most common causes:
- Spasm of the arteriolar walls (e.g. in stress, embolism of pulmonary vessels, pheochromocytoma catecholamine release, in case of acidosis, acute decrease in partial pressure of oxygen in the inspiratory air, altitude hypoxia — reduction of PaO2 (Euler-Lilestrand reflex — constricting response of pulmonary vessels with increased precapillary resistance (pulmonary arterioles coarctation) in response to decreased partial pressure of oxygen in alveolar air). Hypoxia is the most significant factor of vasoconstriction (the most important mediators of vasoconstriction: catecholamines, endothelin, thromboxane A2).
- Obturation of pulmonary microcirculatory vessels (e.g. microthrombus, emboli, hyperplastic endothelium).
- Prelum of the lung arterioles (e.g. by neoplasma, enlarged lymph nodes, increased air pressure in the alveoli and bronchi during an acute fit of coughing, artificial pulmonary ventilation under the positive pressure).
The degree of pulmonary hypertension in case of mountain disease (Euler-Lilestrand reflex) depends on:
- Pa values of oxygen in inspiratory air
- Time spent under hypoxic conditions
- Pulmonary vessels responsiveness
- Severity of haemodynamic changes in the greater circulation
A low ambient temperature that activates the sympathoadrenaline system has a potentiating influence on the vasoconstrictive effect in the high-altitude environments.
Postcapillary hypertension
It is characterized by an abnormal outflow of blood from the vessels into the left atrium and an accumulation of excess blood in the lungs.
The most common causes:
- stegnosis of the mitral valve foramen (for example, as a result of endocarditis)
- pulmonary engorgement
- prelum of the pulmonary veins (for example, by enlarged lymph nodes or by a neoplasma)
- insufficiency of the cardiac muscle contractility of the left ventricle — left ventricular insufficiency (for example, in case of the acute myocardial infarction, arterial hypertension, myocardiodystrophy).
Mixed hypertension
- It can be observed in the following types of pathology:
- congenital heart defects with blood discharge «from left to right» (defects of the interventricular or interatrial septa).
- It is often the result of progression and complications of pre- or post-capillary hypertension. For example, the difficulty of blood outflow from the pulmonary veins to the left atrium, typical for postcapillary hypertension, leads to a reflexory decrease in the lumen of the pulmonary arterioles, typical for precapillary hypertension (Kitaev reflex).
Manifestations:
- signs of the left ventricular and/or right ventricular heart failure (stagnation of blood in venous vessels, ascites, edema, etc.),
- VC decrease,
- hypoxemia and hypercapnia,
- acidosis (respiratory, in case of chronicity it is mixed) [2, p. 214]
Pulmonary hypotension
Pulmonary hypotension is characterized by a persistent decrease in blood pressure in the vessels of the lesser circulation.
The most common causes are:
- Cardiac defects with blood shunting from right to left. At the same time, venous blood shunt occurs; it is discharged into the arterial system (for example, in case of Fallot’s tetralogy, pulmonic regurgitation).
- Hypovolemia of various genesis (for example, in case of long-lasting diarrhea, state of shock, as a result of chronic blood loss).
- Systemic arterial hypotension (for example, in case of collapses or comas). [4, p. 707]
NB! Oxygen inhalation practically does not increase the degree of the blood oxygenation under lung perfusion disorders (the simplest functionality test sample).
In conclusion, it is worth noting that the respiratory diseases traditionally dominate (Table 1) in the structure of the overall morbidity rate of the Russian population, they amount to up to 27.8 % of all registered and 42.7 % of the pathology detected for the first time in life.
Table 1
Statistics on respiratory system morbidity rate in Primorsky Krai
(Data from the Ministry of Health of Russia, calculation of the Russian Statistics Agency)
| Year | 2016 | 2017 | 2018 | 2019 | 2020 |
| All diseases | 115 187 | 114 382 | 114 841 | 114 512 | 111 294 |
| Diseases of the respiratory system | 51 573 | 51 905 | 52 833 | 52 278 | 54 273 |
| Percentage of all diseases | 44.8% | 45.4% | 46% | 45.6% | 48.8% |
Such an increase in morbidity rate is primarily due to the constantly increasing pollution of the environmental air, smoking, and the growing allergization of the population (primarily due to household chemicals). All this determines the relevance of an intensive study of the cause-and-effect relationships of the pathology development in the respiratory system in order to increase the effectiveness of etiotropic and pathogenetic treatment and prevention of relevant diseases that a doctor has to face in daily practice.
References
1. Findlayson, K.D. Pathology in drawings / K.D. Findlayson, B.A. Newell. - Moscow: Laboratory of Knowledge, 2017. - 295 p.2. Novitskiy, V.V. Pathophysiology. Textbook in 2 volumes. / V.V. Novitskiy, O.I. Urazova. - M: GEOTAR-Media, 2018. - 592 p.
3. Litvitskiy, P.F. Pathophysiology. In 2 volumes / P.F. Litvitskiy. - Moscow: GEOTAR-Media, 2016. - 792 p.
4. Litvitskiy, P.F. Clinical pathophysiology / P.F. Litvitskiy. - M.: Practical Medicine, 2017. - 776 p.
